Researchers from The University of Texas MD Anderson Cancer Center have developed a promising antibody therapy, designated as 77A, that significantly enhances the immune response against both blood cancers and solid tumors. This breakthrough was presented by Jun Wei, M.D., Ph.D., at the 67th American Society of Hematology (ASH) Annual Meeting on December 6, 2025, indicating a potential shift in how these cancers are treated.
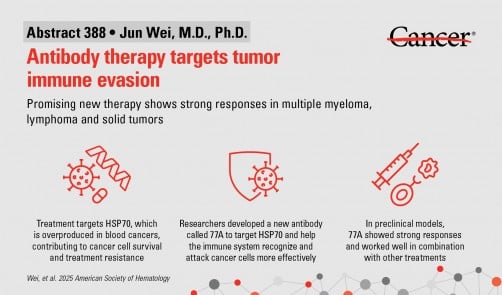
The investigational therapy targets a protein known as HSP70, which plays a critical role in helping tumors evade the immune system. By converting HSP70 into an immune system trigger, 77A activates T cells and natural killer (NK) cells. This activation reshapes the tumor environment, fostering long-lasting immune responses that can combat cancer more effectively.
In laboratory models, 77A demonstrated an ability to overcome resistance to existing treatments, including chemotherapy and radiation, significantly boosting their effects across various tumor types. The findings suggest that 77A could be a game-changing addition to the current arsenal of cancer therapies.
Robert Z. Orlowski, M.D., Ph.D., the study’s principal investigator, expressed optimism about the results: “These findings offer a new pathway to immunotherapy and patient treatment.” The research showed that 77A enhances both innate and adaptive immune responses, improving the ability of immune cells to detect and destroy cancer cells. It has also shown promising potential when combined with other therapies, such as immune checkpoint blockade and adoptive T cell therapy.
The implications of this research could extend far beyond laboratory settings. Early tests involving human immune cells indicated that 77A could enhance immune responses in healthy donors, paving the way for future clinical trials. The development team plans to advance a humanized version of 77A into clinical testing, with the hope that it will become a versatile therapeutic option for patients facing multiple types of cancer.
“This research gives us confidence that 77A could become a versatile immunotherapy,” Orlowski added. As the study progresses, further investigation will focus on its application in clinical settings, assessing its efficacy and safety in human patients.
The study was supported by Blood Cancer United, formerly known as the Leukemia & Lymphoma Society. A comprehensive list of collaborating authors and their disclosures can be found with the published abstract, highlighting the collaborative effort behind this significant advancement in cancer treatment.