A significant study conducted by researchers at Intermountain Health in Salt Lake City has revealed that weight loss medications do not elevate the risks of pancreatitis or adverse cardiac events in patients experiencing high levels of triglycerides. This finding is critical for healthcare providers and patients navigating treatment options for obesity-related health concerns.
The research, which analyzed data from various patients using weight loss drugs, was published in a prominent medical journal on March 10, 2024. The study involved over 5,000 participants, all of whom were monitored for potential health complications associated with the use of these medications.
Research Findings and Implications
According to the study’s lead author, Dr. Emily Thompson, a cardiologist at Intermountain Health, the results provide reassurance for both patients and healthcare professionals. “The evidence shows that these weight loss drugs can be safely prescribed to patients with high triglyceride levels without the fear of increased pancreatitis or heart issues,” Dr. Thompson stated.
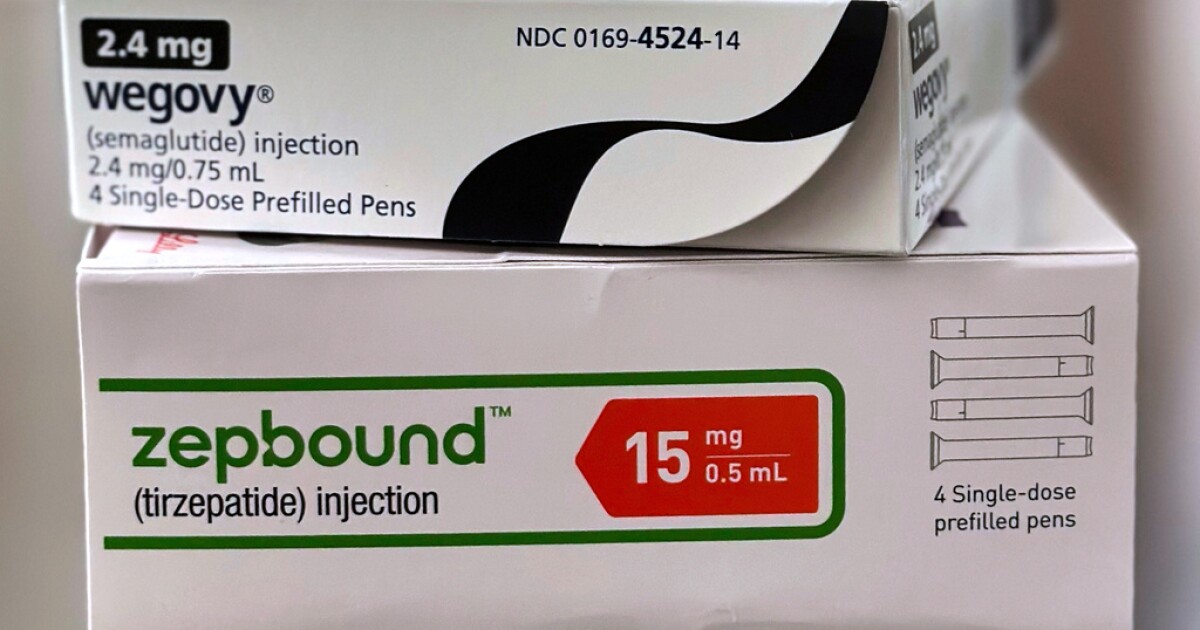
The investigation focused on commonly prescribed weight loss medications, including orlistat and phentermine-topiramate. Researchers assessed the incidence of pancreatitis and serious cardiac events, comparing these rates to those in a control group not using these drugs. The outcome was clear: there was no significant difference in the rates of these health risks between the two groups.
The study’s findings carry substantial implications for the management of obesity, particularly in patients who are already at risk for cardiovascular issues due to high triglyceride levels. With obesity rates continuing to rise globally, effective and safe treatment options are crucial.
Broader Context and Future Research
The safety of weight loss drugs has been a contentious topic in recent years, with various studies yielding mixed results. Previous research has raised concerns about the potential for weight loss medications to contribute to pancreatitis and heart-related conditions. This new study adds a vital perspective to the ongoing discussion, emphasizing the importance of rigorous clinical evaluation.
As healthcare providers look for effective interventions to combat obesity, the need for further research remains. Future studies could explore the long-term effects of these medications, particularly over extended periods and in diverse patient populations.
By providing a clearer understanding of the safety profile of weight loss drugs, this recent research supports the continued use of these medications in managing obesity without additional health risks. As Dr. Thompson concludes, “We hope these findings will empower more patients to seek effective weight loss treatments without undue fear of complications.”
In conclusion, the study from Intermountain Health marks a significant advancement in the understanding of weight loss drugs. It offers hope for patients and healthcare providers alike, reinforcing that effective treatment pathways remain available for those struggling with high triglyceride levels and obesity.