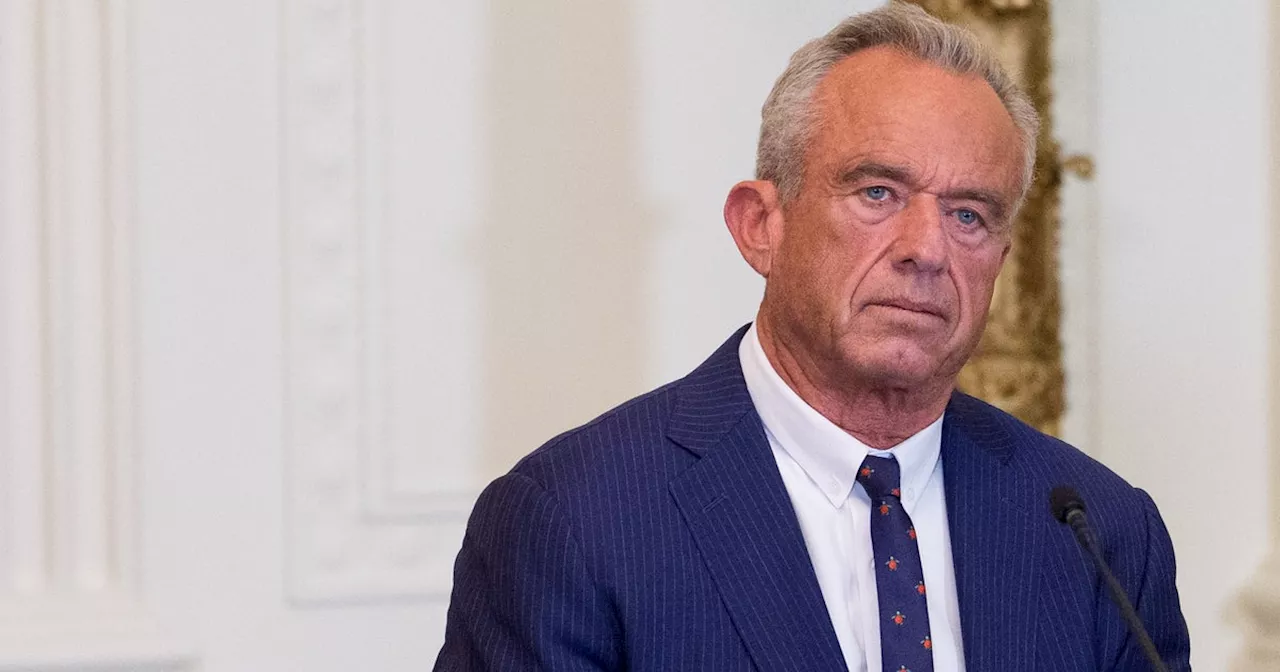
Robert F. Kennedy Jr. recently stated that a ketogenic (keto) diet could “cure” mental illnesses such as schizophrenia. This claim, made during a speech promoting his “Make America Health Again” campaign, has sparked significant debate and requires careful examination.
Kennedy asserted, “We now know that the things that you eat are driving mental illness in this country. And Dr. Pollan, up at Harvard, has cured schizophrenia using keto diets.” He further claimed that recent studies indicate individuals can lose their bipolar diagnosis through dietary changes, emphasizing the importance of consuming “real food” such as protein, fruits, vegetables, and high-fiber grains.
While there is ongoing research into the relationship between diet and mental health, experts caution against overstating the benefits of a keto diet as a definitive treatment. According to Dr. Lippman-Barile, a leading figure in nutritional psychiatry, the current evidence supporting keto diets for mental health is limited. “There is some evidence suggesting a keto diet may be beneficial, but there is not a substantial amount available at this point,” she stated.
Research has explored the potential effects of the keto diet on conditions like bipolar disorder and schizophrenia. However, studies often include small sample sizes and short durations, which makes it difficult to draw firm conclusions. Lippman-Barile pointed out the absence of long-term studies that could provide more comprehensive insights into how such diets affect mental health.
Dr. Ramsey, another expert in the field, noted that dietary interventions can complement traditional treatments but should not replace them. “We are using dietary interventions alongside our evidence-based treatments, not to replace them,” he explained. He highlighted that while some patients with depression have shown improvement with a Mediterranean diet combined with other therapies, calling any diet a “cure” is misleading.
The term “cure” implies a complete resolution of mental health issues, which can be harmful. Mental health diagnoses, when conducted by trained professionals, serve as essential tools for guiding effective treatment strategies. “Recovery is possible with proper treatment, but we should avoid the term ‘cure’ as it can mislead individuals into thinking these conditions can be entirely eradicated,” Ramsey added.
Kennedy’s comments reflect a broader trend in public discourse that favors “natural” solutions over pharmaceutical treatments. This viewpoint aligns with the ideology promoted by his campaign, suggesting that dietary changes can lead to significant improvements in mental health. Yet, according to Lippman-Barile, while diet plays a role, it is not a standalone solution for complex mental health disorders.
Research indicates that individuals with digestive disorders experience higher rates of depression and anxiety, underscoring the intricate relationship between diet and mental health. Lippman-Barile noted that a diet high in ultra-processed foods correlates with increased risks of mental health issues, suggesting that while diet is a factor, it is not the sole cause of mental illness.
Dr. Resch, a psychiatrist and advocate for evidence-based treatments, emphasized the importance of a holistic approach to mental health care. “A variety of interventions, including medication, therapy, and dietary adjustments, are essential for effective treatment,” she said. “Any dietary change is likely to yield better outcomes compared to the standard American diet, which is nutritionally poor.”
Kennedy’s assertion that dietary changes alone can cure serious mental health conditions has drawn criticism for oversimplifying the complexities of these disorders. Experts in the field caution against making sensational claims that could lead individuals to abandon proven treatments in favor of unverified dietary changes.
While the keto diet may hold potential as part of a broader treatment plan for certain conditions, the current consensus among mental health professionals is clear: more research is needed, and claims of a “cure” are premature. As the field of nutritional psychiatry continues to evolve, it remains crucial for advocates and public figures to communicate responsibly about the relationship between diet and mental health.